Blog - Foot Doctor, Chambersburg and McConnellsburg, PA
Managing Peripheral Artery Disease

Peripheral artery disease, or PAD, particularly affects people with type 2 diabetes. Peripheral artery disease is often mistaken for normal aging or arthritis, but in fact it is the result of a build-up of fatty deposits in the arteries that restricts blood supply to the lower limbs and feet. Leg pain during exercise that persists with rest could signal PAD, necessitating evaluation by a podiatrist. Risk factors such as diabetes, smoking, and high cholesterol significantly contribute to PAD. Regular check-ups with a podiatrist, especially for diabetic individuals, are essential for assessing and managing foot health. One side effect of peripheral artery disease is the inability of wounds to heal properly, putting the patient at risk for foot ulcers. Early detection and intervention is essential, as such open wounds can deteriorate into gangrene and increase risk of limb loss if left untreated. For that reason, symptoms like persistent leg pain or slow-healing wounds require prompt medical attention from a podiatrist. If you are experiencing symptoms of peripheral artery disease, it is suggested that you add a podiatrist to your team of healthcare professionals.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Steven Schwartz from Pennsylvania. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in Chambersburg, and Mcconnellsburg, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Definition and Causes of Bunionettes

Bunionettes, also known as tailor's bunions, are bony bumps that develop on the outside of the foot, near the base of the pinky toe. Understanding the definition and underlying causes of these foot deformities is vital for effective management and prevention. Essentially, a bunionette forms when the bone at the base of the fifth toe protrudes outward, often accompanied by the misalignment of the toe joint. This condition is primarily attributed to structural imbalances in the foot, including inherited foot shapes, abnormal foot mechanics, or wearing narrow shoes that compress the toes. Over time, pressure and friction on the affected area can exacerbate the deformity, leading to pain, inflammation, and difficulty wearing certain footwear. While bunions and bunionettes share similar characteristics, they affect different areas of the foot. Bunionettes typically develop on the outer edge of the foot, whereas bunions occur at the base of the big toe. If you have developed a bunion or bunionette, it is suggested that you visit a podiatrist who can determine what the best course of treatment is for you.
If you are suffering from bunion pain, contact Dr. Steven Schwartz of Pennsylvania. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Chambersburg, and Mcconnellsburg, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Understanding Tarsal Tunnel Syndrome

Tarsal tunnel syndrome, or TTS, is a condition characterized by compression of the tibial nerve as it passes through the tarsal tunnel, located on the inner side of the ankle. This compression can lead to a variety of symptoms, including pain, tingling, burning sensations, and numbness along the inner ankle and sole of the foot. Individuals with TTS may also experience weakness in the muscles of the foot, particularly the toes, and may have difficulty standing or walking for prolonged periods of time. Symptoms of TTS often worsen with activity or prolonged standing, and may be worsened by wearing tight shoes or engaging in activities that require repetitive ankle motion. In some cases, the pain and discomfort of TTS can be severe enough to interfere with daily activities and significantly impact quality of life. Early recognition and treatment of tarsal tunnel syndrome is essential to prevent further nerve damage and alleviate symptoms. If you suspect you may have TTS, it is suggested that you confer with a podiatrist who can offer you treatment options that are right for you.
Tarsal tunnel syndrome can be very uncomfortable to live with. If you are experiencing tarsal tunnel syndrome, contact Dr. Steven Schwartz of Pennsylvania. Our doctor can provide the care you need to keep you pain-free and on your feet.
Tarsal Tunnel Syndrome
Tarsal tunnel syndrome, which can also be called tibial nerve dysfunction, is an uncommon condition of misfiring peripheral nerves in the foot. The tibial nerve is the peripheral nerve in the leg responsible for sensation and movement of the foot and calf muscles. In tarsal tunnel syndrome, the tibial nerve is damaged, causing problems with movement and feeling in the foot of the affected leg.
Common Cause of Tarsal Tunnel Syndrome
- Involves pressure or an injury, direct pressure on the tibial nerve for an extended period of time, sometimes caused by other body structures close by or near the knee.
- Diseases that damage nerves, including diabetes, may cause tarsal tunnel syndrome.
- At times, tarsal tunnel syndrome can appear without an obvious cause in some cases.
The Effects of Tarsal Tunnel Syndrome
- Different sensations, an afflicted person may experience pain, tingling, burning or other unusual sensations in the foot of the affected leg.
- The foot muscles, toes and ankle become weaker, and curling your toes or flexing your foot can become difficult.
- If condition worsens, infections and ulcers may develop on the foot that is experiencing the syndrome.
A physical exam of the leg can help identify the presence of tarsal tunnel syndrome. Medical tests, such as a nerve biopsy, are also used to diagnose the condition. Patients may receive physical therapy and prescriptive medication. In extreme cases, some may require surgery.
If you have any questions please feel free to contact our offices located in Chambersburg, and Mcconnellsburg, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Where Are Plantar Warts Found?

Plantar warts, medically termed Verruca plantaris, are common skin growths caused by the human papillomavirus, or HPV. These warts typically appear on the soles of the feet, often in areas subjected to pressure or friction, such as the heels or balls of the feet. Plantar warts often manifest as small, rough, grainy lesions with black dots, or wart seeds, scattered throughout. These black dots are actually tiny blood vessels. While plantar warts are usually harmless, they can cause discomfort or pain, especially when walking or standing. The HPV virus enters the body through small cuts or breaks in the skin, making individuals who frequently walk barefoot in communal areas more susceptible to infection. Treatment options for plantar warts range from remedies like salicylic acid patches or freezing kits to medical procedures performed by podiatrists. Seeking prompt treatment is essential to alleviate symptoms and prevent the spread of plantar warts to other areas of the feet or other individuals. If you have a plantar wart, it is suggested that you schedule an appointment with a podiatrist who can offer the best treatment option for you.
Plantar warts can be very uncomfortable. If you need your feet checked, contact Dr. Steven Schwartz from Pennsylvania. Our doctor will assist you with all of your foot and ankle needs.
About Plantar Warts
Plantar warts are the result of HPV, or human papillomavirus, getting into open wounds on the feet. They are mostly found on the heels or balls of the feet.
While plantar warts are generally harmless, those experiencing excessive pain or those suffering from diabetes or a compromised immune system require immediate medical care. Plantar warts are easily diagnosed, usually through scraping off a bit of rough skin or by getting a biopsy.
Symptoms
- Lesions on the bottom of your feet, usually rough and grainy
- Hard or thick callused spots
- Wart seeds, which are small clotted blood vessels that look like little black spots
- Pain, discomfort, or tenderness of your feet when walking or standing
Treatment
- Freezing
- Electric tool removal
- Laser Treatment
- Topical Creams (prescription only)
- Over-the-counter medications
To help prevent developing plantar warts, avoid walking barefoot over abrasive surfaces that can cause cuts or wounds for HPV to get into. Avoiding direct contact with other warts, as well as not picking or rubbing existing warts, can help prevent the further spread of plantar warts. However, if you think you have developed plantar warts, speak to your podiatrist. He or she can diagnose the warts on your feet and recommend the appropriate treatment options.
If you have any questions please feel free to contact our offices located in Chambersburg, and Mcconnellsburg, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes and Nature of Morton's Neuroma
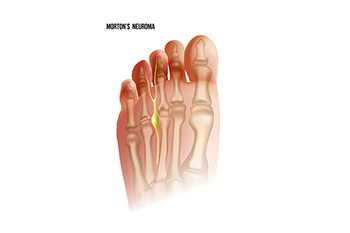
Morton's neuroma, a common foot condition, occurs when a nerve in the ball of the foot becomes thickened and inflamed, leading to pain and discomfort. This condition typically affects the area between the third and fourth toes but can also occur between other toes. The exact cause of Morton's neuroma is not always clear, but it often develops due to repetitive stress or irritation on the nerve, such as wearing tight or high-heeled shoes that compress the forefoot. Activities that involve repetitive pressure on the ball of the foot, such as running or participating in high-impact sports, can also contribute to the development of Morton's neuroma. Additionally, foot deformities like bunions, hammertoes, or flat feet may increase the risk. Understanding the underlying causes of Morton's neuroma is important for effective management and prevention strategies, which may include wearing supportive footwear, using orthotic inserts, and avoiding activities that exacerbate symptoms. If you have pain in this part of your foot, it is strongly suggested that you are under the care of a podiatrist who can accurately diagnose and treat Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Steven Schwartz of Pennsylvania. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our offices located in Chambersburg, and Mcconnellsburg, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Diagnosis and Stretches for Plantar Fasciitis Relief

Plantar fasciitis, a common cause of heel pain, occurs when the thick band of tissue running along the bottom of the foot becomes inflamed. Diagnosing this condition typically involves a thorough physical examination by a podiatrist, focusing on the affected foot's tenderness and range of motion. Imaging tests such as X-rays or MRI scans may also be utilized to rule out other possible causes of heel pain and confirm the diagnosis. Once diagnosed, incorporating stretching exercises into a daily routine can help alleviate symptoms and promote healing. Simple stretches targeting the calf muscles and the plantar fascia itself, such as calf stretches, towel stretches, and plantar fascia stretches can effectively reduce tightness and discomfort. These stretches should be performed gently and consistently to gradually improve flexibility and reduce strain on the affected tissues. In addition to stretching, lifestyle modifications may be recommended to manage plantar fasciitis and restore foot health. If you have heel pain, it is strongly suggested that you are under the care of a podiatrist who can offer you treatment options.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Steven Schwartz from Pennsylvania. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our offices located in Chambersburg, and Mcconnellsburg, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Nurturing Your Feet With a Foot Care Routine

Your feet bear the weight of your bodiy and facilitate movement with every step. To ensure their health and well-being, it is important to establish a consistent foot care routine. Start by cleaning your feet daily with mild soap and warm water, paying special attention to the spaces between your toes. Regularly trimming toenails straight across helps prevent ingrown toenails and infections. Moisturizing your feet with a hydrating lotion or cream keeps the skin soft and supple, preventing dryness and cracks. Additionally, wearing properly fitting shoes with adequate support and cushioning can help prevent discomfort and reduce the risk of foot problems, such as bunions or plantar fasciitis. Finally, incorporating gentle stretches and exercises into your routine promotes flexibility and strength in the muscles and ligaments of the feet. If you are experiencing any foot problems, or are seeking additional information about effective foot care routine strategies, it is suggested that you consult a podiatrist.
Everyday foot care is very important to prevent infection and other foot ailments. If you need your feet checked, contact Dr. Steven Schwartz from Pennsylvania. Our doctor can provide the care you need to keep you pain-free and on your feet.
Everyday Foot Care
Often, people take care of their bodies, face and hair more so than they do for their feet. But the feet are a very important aspect of our bodies, and one that we should pay more attention to. Without our feet, we would not be able to perform most daily tasks.
It is best to check your feet regularly to make sure there are no new bruises or cuts that you may not have noticed before. For dry feet, moisturizer can easily be a remedy and can be applied as often as necessary to the affected areas. Wearing shoes that fit well can also help you maintain good foot health, as well as making it easier to walk and do daily activities without the stress or pain of ill-fitting shoes, high heels, or even flip flops. Wearing clean socks with closed shoes is important to ensure that sweat and bacteria do not accumulate within the shoe. Clean socks help to prevent Athlete’s foot, fungi problems, bad odors, and can absorb sweat.
If you have any questions please feel free to contact our offices located in Chambersburg, and Mcconnellsburg, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Common Signs of Poor Foot Circulation

Effective circulation is essential for maintaining optimal foot health and overall well-being. Poor foot circulation, often overlooked, can lead to various discomforts and complications if left unaddressed. Common signs of inadequate circulation in the feet include persistent coldness or numbness, particularly in the toes and lower extremities. Individuals may also experience tingling sensations, known as paresthesia or pins and needles, indicative of reduced blood flow. Swelling, discoloration, and slow-healing wounds or ulcers on the feet are additional signs that circulation may be compromised. Cramping or muscle weakness in the legs and feet, especially during physical activity, can also signal poor circulation. In severe cases, individuals may develop peripheral artery disease, abbreviated PAD, which is a condition characterized by narrowed arteries that restrict blood flow to the extremities. If you are experiencing poor foot circulation, it is suggested that you are under the care of a podiatrist who can help you to manage this condition.
Poor circulation is a serious condition and needs immediate medical attention. If you have any concerns with poor circulation in your feet contact Dr. Steven Schwartz of Pennsylvania. Our doctor will treat your foot and ankle needs.
Poor Circulation in the Feet
Poor blood circulation in the feet and legs is can be caused by peripheral artery disease (PAD), which is the result of a buildup of plaque in the arteries.
Plaque buildup or atherosclerosis results from excess calcium and cholesterol in the bloodstream. This can restrict the amount of blood which can flow through the arteries. Poor blood circulation in the feet and legs are sometimes caused by inflammation in the blood vessels, known as vasculitis.
Causes
Lack of oxygen and oxygen from poor blood circulation restricts muscle growth and development. It can also cause:
- Muscle pain, stiffness, or weakness
- Numbness or cramping in the legs
- Skin discoloration
- Slower nail & hair growth
- Erectile dysfunction
Those who have diabetes or smoke are at greatest risk for poor circulation, as are those who are over 50. If you have poor circulation in the feet and legs it may be caused by PAD and is important to make changes to your lifestyle in order to reduce risk of getting a heart attack or stroke. Exercise and maintaining a healthy lifestyle will dramatically improve conditions.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions please feel free to contact our offices located in Chambersburg, and Mcconnellsburg, PA . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.