May 2024
Geriatrics and Podiatry
Bone density loss, dry skin, poor circulation, and rough and brittle nails are some of the common problems that can occur as people age. The effect that these problems has on foot health should be of particular concern in comprehensive geriatric care.
Feet that are diseased or injured have a negative effect on overall health and safety. Painful feet limit a person’s willingness and ability to stay active. Poor foot health can also cause gait change, which can lead to falls and accidents. Even though recovery time from health problems naturally slows as we age, many foot problems can be avoided altogether with regular prophylactic care.
Feet should be thoroughly washed in warm water daily. Care must be taken to dry the feet well, making sure to dry between and under the toes. Any left-over moisture can cause problems like foot fungus. After cleaning feet carefully check for problems such as cracked skin, bruises, swelling, cuts, corns, or other irregularities.
Examine toenails for ingrown, jagged, or split nails. Long toenails should be cut straight across. Never cut toenails at an angle or down the side as this may lead to ingrown nails.
Cracked and dry feet should be treated once or twice a day with a non-greasy moisturizer. Rub the moisturizer into the skin and allow it to dry before putting on socks and shoes. Sweaty feet can be dusted with a small amount of talcum powder. Avoid putting talcum directly into shoes as this may make feet slip within the shoe and cause a serious fall.
Wear clean dry socks each day. Not only do clean socks feel better on the feet, but socks worn for longer periods may harbor disease and odor-causing bacteria. Socks should not be tight around the top as they can leave marks on the leg. Socks that are too small can bring about bruising caused by pressure against the toes.
Wear comfortable and well-fitting shoes. If possible, consult a professional footwear specialist when purchasing shoes. Do not walk around barefoot as this exposes the feet to possible injury and bacteria.
Good foot health allows a more active lifestyle, which improves blood flow. Good circulation aids in recovery from injury or illness. It is also important for maintaining overall health.
Serious health problems can manifest themselves as symptoms in the feet. The elderly should seek professional help from a podiatrist if experiencing foot problems like tingling, numbness, pain, infection, or a sore that does not heal. Taking care of these problems right away can prevent the development of severe cases.
Foot Problems in Seniors

As people age, maintaining foot health becomes vital, but yet often overlooked. Older adults commonly face several foot problems that can significantly impair their mobility and quality of life. These issues can include arthritis, which leads to joint pain and deformity, diabetes-related complications like neuropathy, which increases the risk of foot ulcers, and circulatory problems that slow healing and increase infection risks. Other common concerns are plantar fasciitis, bunions, hammertoes, and fungal infections, which become more prevalent with age due to changes in skin elasticity and foot structure. Preserving foot health is essential for seniors as it supports mobility, balance, and overall independence. Prevention plays a key role and involves proper foot hygiene, well-fitting, supportive footwear, and regular foot checks to identify problems early. Given the complexities of foot care in older age, if you are a senior, it is suggested that you schedule regular appointments with a podiatrist who can provide tailored advice and treatment, helping to maintain foot health and enhance quality of life.
If you need your feet checked, contact Dr. Steven Schwartz of Pennsylvania. Our doctor will attend to all of your foot and ankle needs and provide you with quality treatment.
Geriatrics and Podiatry
When people age, some common issues that may occur are bone density loss, dry skin, poor circulation, and rough brittle nails. These issues may also affect your foot health if the necessary steps are not taken to alleviate the problems.
It is important to take care of your feet because feet that are injured or diseased can affect your overall health. Having painful feet hinders your ability to do daily activities or may decrease your willingness to do the things that you need to do.
Visiting Your Geriatrician
As we age, health problems become more likely, so it is essential to visit your doctor for check-ups to ensure that you are doing the best you can to take care of your health. It is recommended to check your feet frequently for any possible cuts, bruises, swelling, corns or any other irregularities.
Taking Care of Elderly Feet
Cracked or dry feet can be treated by applying moisturizer often. It is also important not to wear old socks because the older the sock is, the higher the possibility there will be that there is bacteria there. Wear fresh socks and make sure they fit properly.
Proper foot health means that you can have a more active lifestyle and you will not be bogged down by pain. Foot health also leads to good circulation, which is paramount for overall health.
If you have any questions, please feel free to contact our offices located in Chambersburg, and Mcconnellsburg, PA . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Foot Pain
Our feet are arguably the most important parts of our bodies because they are responsible for getting us from place to place. However, we often don’t think about our feet until they begin to hurt. If you have pain in your feet, you need to first determine where on the foot you are experiencing it to get to the root of the problem. The most common areas to feel pain on the foot are the heel and the ankle.
Heel pain is most commonly attributed to a condition called plantar fasciitis. Plantar fasciitis occurs when the plantar fascia, which is the band of tough tissue connecting the heel bone to the toes becomes inflamed. Plantar fasciitis pain is usually worse in the morning, and it tends to go away throughout the day. If you have plantar fasciitis, you should rest your foot and do heel and foot muscles stretches. Wearing shoes with proper arch support and a cushioned sole has also been proven to be beneficial.
Some common symptoms of foot pain are redness, swelling, and stiffness. Foot pain can be dull or sharp depending on its underlying cause. Toe pain can also occur, and it is usually caused by gout, bunions, hammertoes, ingrown toenails, sprains, fractures, and corns.
If you have severe pain in your feet, you should immediately seek assistance from your podiatrist for treatment. Depending on the cause of your pain, your podiatrist may give you a variety of treatment options.
Addressing Foot Pain

Foot pain comes in various forms, each signaling potential underlying issues that should not be disregarded. Plantar fasciitis, a common cause of heel pain, results from inflammation of the plantar fascia ligament, often due to overuse or improper footwear. Morton's neuroma, characterized by a sharp, burning sensation in the ball of the foot, stems from the thickening of the tissue around a nerve, typically caused by pressure or irritation. Bunions, hallux rigidus, and stress fractures are additional examples of foot conditions that can cause discomfort and affect mobility. Ignoring foot pain can lead to exacerbated symptoms, decreased quality of life, and even chronic conditions that require more invasive treatments. Proper diagnosis and timely intervention are essential for addressing foot pain and preventing long-term complications. Consulting a podiatrist can help identify the underlying causes and develop an effective treatment plan to alleviate discomfort and promote foot health. If you have any foot pain, it is suggested that you confer with this type of doctor who can provide a diagnosis and treatment.
Foot Pain
Foot pain can be extremely painful and debilitating. If you have a foot pain, consult with Dr. Steven Schwartz from Pennsylvania. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Causes
Foot pain is a very broad condition that could be caused by one or more ailments. The most common include:
- Bunions
- Hammertoes
- Plantar Fasciitis
- Bone Spurs
- Corns
- Tarsal Tunnel Syndrome
- Ingrown Toenails
- Arthritis (such as Gout, Rheumatoid, and Osteoarthritis)
- Flat Feet
- Injury (from stress fractures, broken toe, foot, ankle, Achilles tendon ruptures, and sprains)
- And more
Diagnosis
To figure out the cause of foot pain, podiatrists utilize several different methods. This can range from simple visual inspections and sensation tests to X-rays and MRI scans. Prior medical history, family medical history, and any recent physical traumatic events will all be taken into consideration for a proper diagnosis.
Treatment
Treatment depends upon the cause of the foot pain. Whether it is resting, staying off the foot, or having surgery; podiatrists have a number of treatment options available for foot pain.
If you have any questions, please feel free to contact our offices located in Chambersburg, and Mcconnellsburg, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Managing Peripheral Artery Disease
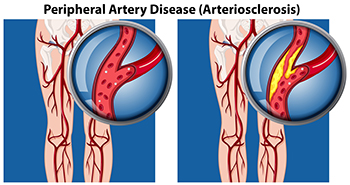
Peripheral artery disease, or PAD, particularly affects people with type 2 diabetes. Peripheral artery disease is often mistaken for normal aging or arthritis, but in fact it is the result of a build-up of fatty deposits in the arteries that restricts blood supply to the lower limbs and feet. Leg pain during exercise that persists with rest could signal PAD, necessitating evaluation by a podiatrist. Risk factors such as diabetes, smoking, and high cholesterol significantly contribute to PAD. Regular check-ups with a podiatrist, especially for diabetic individuals, are essential for assessing and managing foot health. One side effect of peripheral artery disease is the inability of wounds to heal properly, putting the patient at risk for foot ulcers. Early detection and intervention is essential, as such open wounds can deteriorate into gangrene and increase risk of limb loss if left untreated. For that reason, symptoms like persistent leg pain or slow-healing wounds require prompt medical attention from a podiatrist. If you are experiencing symptoms of peripheral artery disease, it is suggested that you add a podiatrist to your team of healthcare professionals.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Steven Schwartz from Pennsylvania. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our offices located in Chambersburg, and Mcconnellsburg, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
Definition and Causes of Bunionettes

Bunionettes, also known as tailor's bunions, are bony bumps that develop on the outside of the foot, near the base of the pinky toe. Understanding the definition and underlying causes of these foot deformities is vital for effective management and prevention. Essentially, a bunionette forms when the bone at the base of the fifth toe protrudes outward, often accompanied by the misalignment of the toe joint. This condition is primarily attributed to structural imbalances in the foot, including inherited foot shapes, abnormal foot mechanics, or wearing narrow shoes that compress the toes. Over time, pressure and friction on the affected area can exacerbate the deformity, leading to pain, inflammation, and difficulty wearing certain footwear. While bunions and bunionettes share similar characteristics, they affect different areas of the foot. Bunionettes typically develop on the outer edge of the foot, whereas bunions occur at the base of the big toe. If you have developed a bunion or bunionette, it is suggested that you visit a podiatrist who can determine what the best course of treatment is for you.
If you are suffering from bunion pain, contact Dr. Steven Schwartz of Pennsylvania. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Chambersburg, and Mcconnellsburg, PA . We offer the newest diagnostic and treatment technologies for all your foot care needs.